Abstract
Background
Allogeneic hematopoietic stem cell transplantation (alloSCT) is a curative therapeutic modality in acute myeloid leukemia (AML). While numerous studies have confirmed the benefit of alloSCT - improved overall survival (OS) and reduced cumulative incidence of relapse (CIR) - restricted mainly to the intermediate and high-risk groups, indications for alloSCT are becoming more restricted over time. Residual disease (RD) monitoring has been proven to be highly predictive of long-term AML outcomes and is now used commonly to guide ongoing therapy decisions. RD-based guidelines in AML propose the use of multiparameter flow cytometry-based RD (FRD) analyses in patients whose disease cannot be followed by molecular means (e.g. CBF AML, APL, NPM1-mutated AML).
Methods
We performed a retrospective review to evaluate the potential therapeutic benefit of alloSCT in AML patients who achieved first complete remission (CR1) and to further define this benefit based on the FRD status at remission. We performed a time-dependent analysis using the covariate of time-to-alloSCT as the primary endpoint of the study. The Mantel-Byar method was applied to compare time to event between the alloSCT and non-transplant groups, addressing time bias concerns that occur with alloSCT studies, according to the FRD status at the time of remission.
Results
The FRD assay has been part of our standard of care since 2015 with a sensitivity of 0.1%. The cohort analyzed included 435 patients treated between 2015 and 2018, of which 336 patients had FRD assessment at CR1. The patients were risk classified using the European Leukemia Network (ELN) 2017 classification which integrates cytogenetic and mutational analyses. The proportion of patients with positive FRD (RDpos) at the post-induction time-point was 35.1% (n=118). Negative residual disease (RDneg) status after induction occurred more frequently in de novo, favorable risk, and NPM1-mutated AMLs, than in the adverse risk or secondary AML groups.
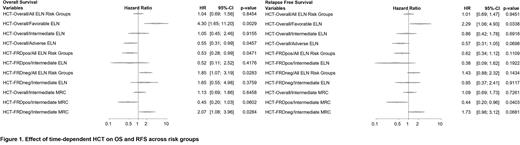
Overall, across all ELN 2017 groups, the impact of alloSCT was neutral for both OS and relapse free survival (RFS). A potential impact of alloSCT could be discerned, however, when patients were grouped by FRD status at CR assessment. Overall, in the RDpos group, alloSCT improved OS and RFS, while not benefitting the RDneg group. The impact of alloSCT was defined further by considering ELN 2017 risk groups, with an OS/RFS benefit observed in adverse risk patients (n=186; HR for OS 0.55 [0.31-0.99]; p=0.05); HR for RFS 0.57 [0.31-1.05], p=0.07), while an increased risk of death or of an RFS event was seen in favorable risk patients (n=151; HR for OS 4.3 [1.65-11.2], p=0.003; HR for RFS 2.29 [1.07-4.93], p=0.03).
In the ELN 2017 intermediate risk patients (n=98), a survival benefit of alloSCT was not seen (HR for OS 1.05 [0.45-2.46], p=0.92; HR for RFS 0.86 [0.42-1.78], p=0.69), although alloSCT was associated with a lower CIR (HR 0.43 [0.20-0.90], p=0.03). However, when only RDpos patients were considered (n=27), trends towards benefit from alloSCT in OS (HR 0.52 [0.11-2.52], p=0.42), RFS (HR 0.38 [0.09-1.62], p=0.19), and CIR (HR 0.44 [0.07-2.72], p=0.38) were observed. In RDneg patients (n=53), alloSCT was associated only with a lower CIR (HR 0.18 [0.05-0.66], p=0.01).
We then re-analyzed the data using the older UK-MRC risk classification of AML based exclusively on cytogenetics at diagnosis. This approach increased the patients in the intermediate group from 98 (ELN 2017) to 298 (UK-MRC). When using UK-MRC, an RFS benefit from alloSCT was observed for intermediate risk RDpos patients (n=211; HR 0.44 [0.20-0.96], p=0.04). Trends for benefit in OS (HR 0.45 [0.19-1.03], p=0.06) and CIR (HR 0.45 [0.20-1.04], p=0.06) were observed as well. In RDneg patients, however, an RFS/CIR benefit of alloSCT was not observed, while inferior OS was seen in the alloSCT group from increased non-relapse mortality.
Conclusion
Our data underscore the established benefit of alloSCT in adverse risk AML and suggest a potential benefit of this treatment modality in RDpos intermediate risk patients, thus confirming the utility of ongoing RD assessment in AML. Our results also indicate that ongoing sophistication in AML risk assignment, based on mutational profile at diagnosis, influences the potential benefit of alloSCT. Further studies are needed to better define the subgroup of RDpos intermediate risk patients who may benefit from alloSCT.
Disclosures
Gupta:AbbVie: Consultancy, Other: Participation on a Data Safety or Advisory board; Constellation Pharmaceuticals, Inc., a MorphoSys Company: Consultancy, Honoraria; Roche: Other: Participation on a Data Safety or Advisory board; BMS Celgene: Consultancy, Honoraria, Other: Participation on a Data Safety or Advisory board; Sierra Oncology: Consultancy; Pfizer: Consultancy, Other: Participation on a Data Safety or Advisory board; Novartis: Consultancy, Honoraria. Schuh:Jazz Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees; GlycoMimetics: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Astellas: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees; Phebra: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Membership on an entity's Board of Directors or advisory committees; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Servier: Membership on an entity's Board of Directors or advisory committees; Teva Pharmaceutical Industries: Membership on an entity's Board of Directors or advisory committees. Kim:Merck: Consultancy; Sanofi: Consultancy, Honoraria; Paladin: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; BMS: Research Funding; Novartis: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.